Antibiotics play a key role in human health by helping us to combat bacterial infection. Unfortunately, bacteria are rapidly evolving resistance to multiple antibiotics, and antibiotic-resistant infections now cause >1 million deaths worldwide per year.
With a small numbers of ‘last-resort’ antibiotics available, it is very important that we understanding how quickly common bacterial pathogens can develop resistance to them. To do this, researchers are investigating the processes that drive the rise, and fall, of resistance in pathogen populations, which is key to overcoming the rise in antimicrobial resistance (AMR).
A recent study published in Cell Reports today by Craig MacLean and colleagues at the Department of Biology, reveals insights into how populations of a bacterium called Pseudomonas respond to being treated with the antibiotic Colistin. Pseudomonas is a bacterium that commonly causes lung infections that can be caught whilst in hospital, whilst Colistin is used as a 'last resort' antibiotic for patients who have developed multi-drug resistant infections.
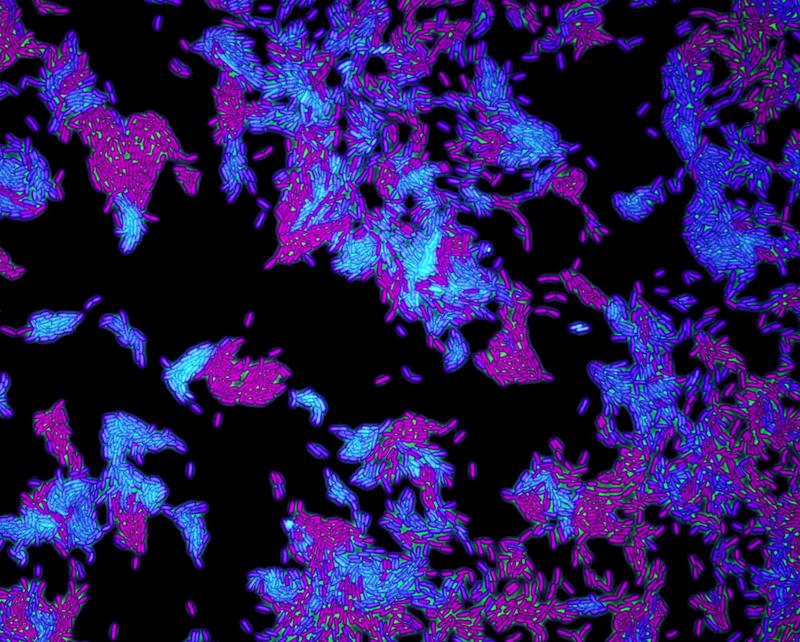
Pseudomonas bacteria under a microscope. Image by Sean Booth
The researchers cultured over 900 populations of Pseudomonas and treated them with Colistin – then, by counting bacteria and sequencing their genome, they could assess how quickly the different populations evolved resistance to the antibiotic and what the genetic mutation was that causes the resistance.
They found that even Pseudomonas infections very easily evolved resistance to this last-resort antibiotic – as a result of a gene that mutates a rate 1,000 times higher than the ‘normal’ background rate of mutation. Mutations in this gene, known as pmrB, is what allowed the bacteria to evolve resistance.
Researchers speculate that the reason for this fast mutation rate is because the pmrB gene is associated with the human immune system. A fast mutation rate might allow this bacterium to adapt to the fluctuating changes in our immune system, in order for the bacterium to survive.
This work is very important as it shows that bacteria can evolve resistance to a clinically vital antibiotic at a much higher rate than expected. This may explain why Colistin has a high failure rating when used to treat patients.
Fortunately, the research did reveal some good news: the pathogen populations really quickly lose resistance when you take the antibiotic away as a consequence of this high mutation rate. This information may help to inform the frequency of use of Colistin in a clinical setting.
Researchers think that the discovery of pmrB’s fast mutations rate is only the tip of iceberg, and plan to investigate other mechanisms in this bacterial infection that allow it to generate high rates of AMR.
Professor Craig MacLean, Professor of Evolution and Microbiology, says:
Our work has shown that a gene involved in resistance to a last resort antibiotic mutates at an incredibly high rate, allowing bacteria to quickly evolve antibiotic resistance.
Our research suggests that, for this particular case, selective pressures generated by this gene’s association with the immune system may have driven the evolution of extra-fast mutation rate, that be quickly evolving to make bacteria resistant to antibiotics.
To read more about this research, published in the Journal of Cell Report, please visit https://www.cell.com/cell-reports/fulltext/S2211-1247(22)00711-2.